Today we spoke with Dmitry Broshkov, a leading expert in digital healthcare software design and architecture, to discuss the importance, implementation, and future of patient-centred design systems. He has built healthcare digital products for many startups, and non-profit organisations such as MSF (Médecins Sans Frontières) and was involved as Fractional CTO for J&J’s (Johnson & Johnson) internal product.
In this interview, we will discuss why patient-centric design systems are not just a trend, but a necessary shift towards more empathic, efficient, and technologically integrated solutions in healthcare. We will look at the challenges faced, the innovative solutions offered, and the principles that guide the creation of environments where patient well-being is paramount.
Can you explain what patient-centred design systems are and what are the first steps in creating a patient-centred design system?
Patient-centric design is an approach that involves the active participation of patients, healthcare providers, and clinicians in the design process. It goes beyond the traditional focus on efficiency and cost-effectiveness to incorporate elements that enhance the patient experience.
Let’s take a closer look at the stages of developing a patient-centred system:
Image 1: Phases of Developing a patient-centred system
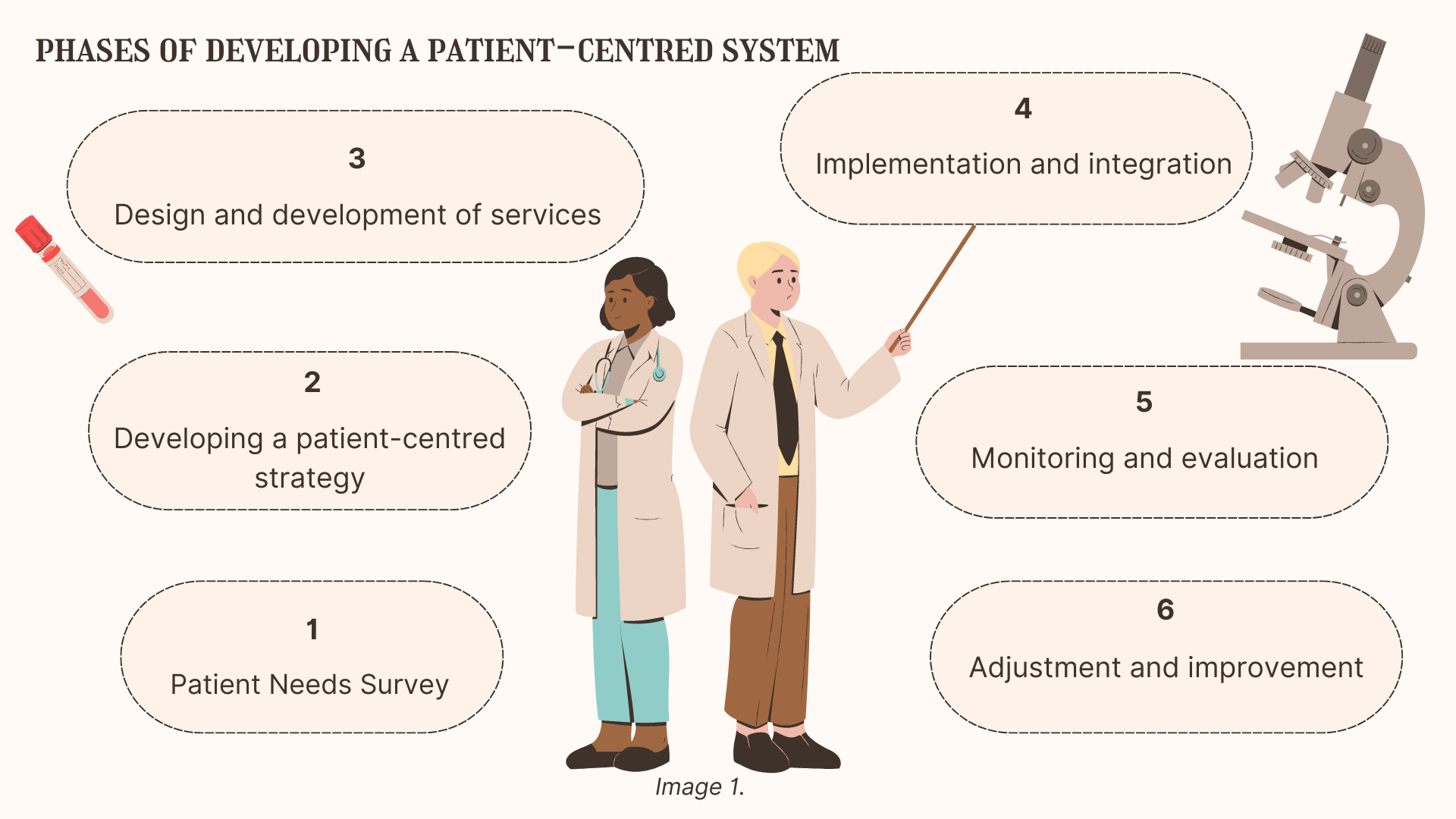
It all starts with understanding patients’ needs, expectations and concerns through methods such as questionnaires, interviews and analysing patient data. A strategy is then developed that includes improving access to services, personalising care and improving communication, ensuring that patients are treated with respect and actively involved in their care.
How do you integrate and evaluate these patient-centred systems into existing health systems?
After developing outcome-based health services, we implement and integrate these software services, making sure that they fit seamlessly into the existing system. It is very important to monitor and evaluate the effectiveness of these implementations, using feedback from both patients and health workers to continually adjust and improve the system.
Can you give an example of an innovative project that embodies patient-centred design?
A good example is the SmartDC project where I am currently involved in the CTO role. The core of the SmartDC project is an EMR system that combines artificial intelligence assistants with electronic medical records. This innovation improves the efficiency of medical consultations around the world, making healthcare more accessible and patient care more personalised and proactive.
The SmartDC AI assistant concept was developed in response to the need to address several critical challenges faced by doctors and therapists in their daily practice. These include improving the quality of medical consultations, the inability of some countries to provide quality healthcare, and automating record keeping by automating the routine processes of making entries into patient profiles.
Our goal is to hand over all the routine processes of making patient profile entries to AI assistants. Doctors will then be able to focus more on patient care and increase their productivity.
Here are some real cases which solve SmartDC platform:
Firstly, summaries are generated by artificial intelligence. After each appointment, the artificial intelligence model generates a detailed summary and automatically updates the patient record by adding all necessary information, dates and potential next steps.
In addition, a computer vision model analyses the lab results uploaded to the EMR translates them into the text format and adds this information to the medical record. This is especially useful later on for creating case summaries and case reports. Also, it simplifies search and finding necessary lab results and gives other AI models to analyse this data for further actions.
Finally, voice recognition allows physicians to dictate notes during an appointment, which are then automatically added to the patient’s profile which also helps to increase productivity and synchronize updated information patient profiles.
As a result, using our generative AI models, we can show doctors a summary based on the patient’s case history, with possible next steps and recommendations.
All these innovative tools greatly simplify the work of doctors, minimise the risks of human error and increase the efficiency of medical record keeping. I want to emphasise that our innovations impact both doctors and patients. For clinicians and physicians, technology reduces the burden of administrative tasks, allowing them to focus more on patient care. On the other hand, patients benefit from improved access to quality care, faster diagnosis and personalised treatment plans, even in remote areas.
Another example of such a project, where I am also CTO, is the 2BWell platform. This platform is a mental health AI chatbot and support system specifically designed for people affected by the military conflict. It provides psychological support through an integrated digital platform that includes an artificial intelligence-based chatbot, direct communication with counsellors and community-building features tailored to the cultural and linguistic needs of the Ukrainian population.
The project was motivated by the growing mental health crisis among millions of Ukrainians, exacerbated by the ongoing conflict. To address this issue, 2BWell offers key features such as an artificial intelligence chatbot called ‘Uncle Zen’ for personalised support, instant connection to trained volunteers and professional therapists, and community building for peer support. All of these elements together provide accessible, immediate and culturally sensitive support aimed at alleviating the mental stress faced by users.
We also implemented automated and continuous engagement with its user base through regular feedback collection, ensuring responsiveness to their evolving needs.
The platform has quite rigorous outcome monitoring to evaluate the impact of its features, like the AI chatbot and counselling services, on users’ mental health.
In addition, we have periodic inclusive design workshops that can help in co-designing updates with users, ensuring the platform remains culturally and linguistically relevant.
This approach helps us maintain the platform’s relevance and effectiveness, enhancing its capacity to offer immediate, accessible, and empathetic support to those affected by military conflict, thereby truly embodying a patient-centred design.
What challenges do you face in implementing patient-centric design systems?
The introduction of new technologies in healthcare is often met with serious resistance. This inertia is a serious problem, especially in systems entrenched in traditional ways of working. So one of the biggest obstacles is, of course, the resistance to innovation inherent in the healthcare system.
A particular focus is on cybersecurity. By establishing robust R&D and QA departments, they ensure that digital health solutions meet the highest standards of data protection. This commitment is vital in gaining the trust of both healthcare professionals and patients, making them more open to adopting new technologies.
In addition, regulatory compliance plays a critical role in this strategy. Need to navigate the complex landscape of local compliance and regulatory standards by integrating these requirements into the very structure of solutions. This proactive approach not only protects patient data, but also ensures compliance with local and international regulations, ensuring that our innovations are implemented without challenges or legal hurdles.
In addition, health systems are challenged by the volume and quality of data: reports indicate that a significant portion of healthcare spending is wasted due to inefficiencies caused by poor data interoperability. For example by National Center for Biotechnology Information, in 2023 states that about 60% of health systems receive duplicate or incomplete data, and 32% of diagnostic laboratories do not participate in health information exchange at all. Overcoming these challenges requires a strategic approach that includes both short-term measures, such as better regulation, and long-term strategies, such as fostering a culture of transparency and collaboration.
Also, let is take a look at the main types of barriers, such as resistance to change, scepticism, lack of resources, lack of training and organisational rigidity, and potential solutions that can help overcome these barriers and ease the transition to a new way of working. This tool will be useful to managers and teams seeking to optimise processes within an organisation with a focus on patient satisfaction.
Table 1: Organisational barriers to a patient-centred approach.
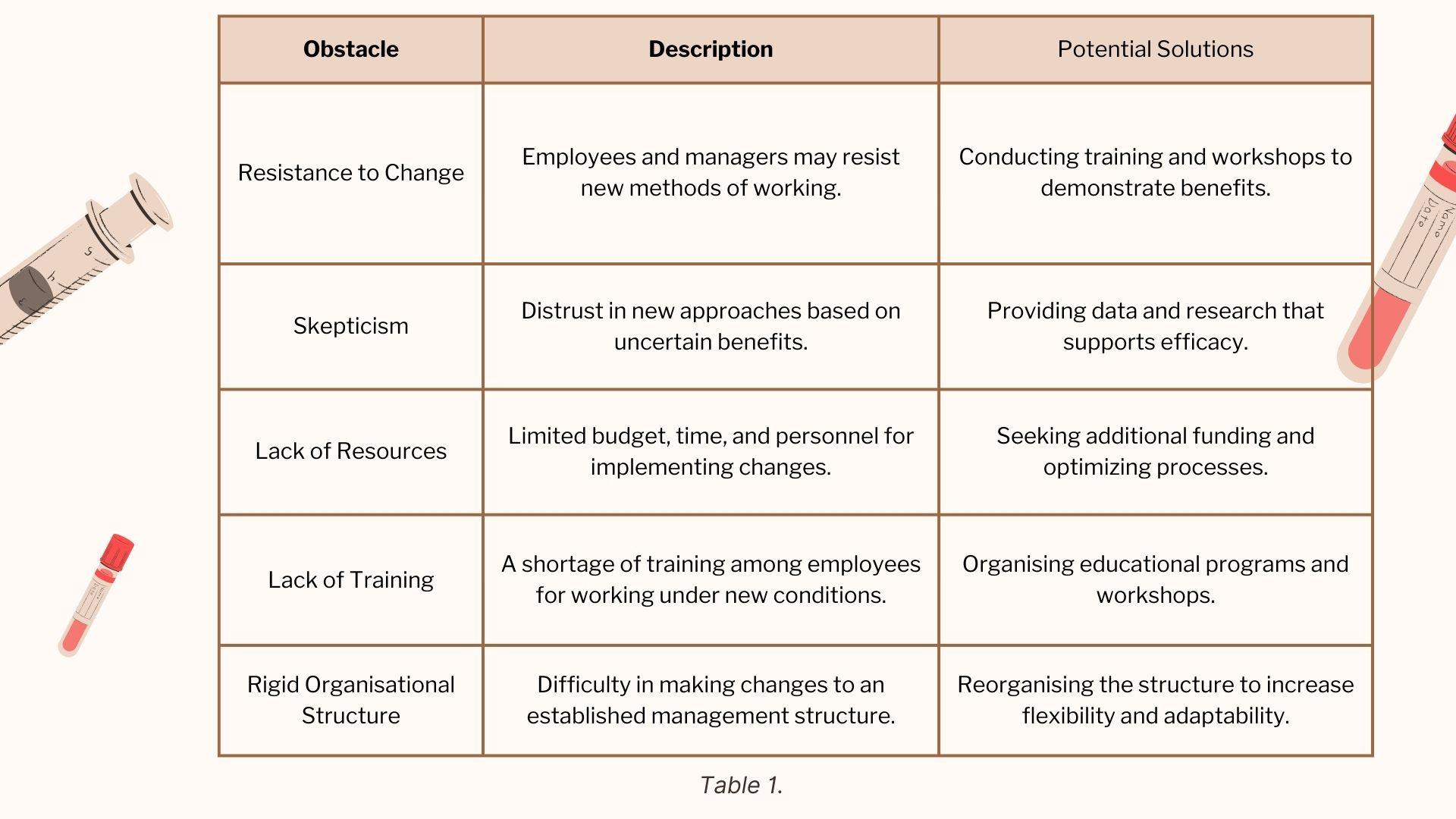
This table describes the key organisational barriers that may arise when trying to move to a patient-centred approach. The table outlines the main types of barriers such as resistance to change, scepticism, lack of resources, lack of training, and rigidity of the organisational structure. For each obstacle, a detailed description is provided to help understand the reasons for its occurrence. The table also identifies potential solutions that can help overcome these barriers and ease the transition to a new way of working. This tool will be useful for managers and teams looking to optimise processes within an organisation with a focus on patient satisfaction.
What are some of the key principles underpinning patient-centred design?
The key principles include empathy, collaboration, accessibility, adaptability and an aesthetic approach to healthcare facilities. Each principle ensures that healthcare services are not only functional but also welcoming and responsive to the diverse needs of patients.
How do continuous improvement and technology affect the future of patient-centred design?
Continuous improvement is vital. For example, we at SmartDC and 2BWell are constantly looking for new ways to improve the quality of care through artificial intelligence and machine learning solutions. In addition, the future may see greater adoption of wearable technology to enable real-time health tracking and empower patients to take an active role in managing their health.
Finally, what does the future of patient-centred design systems look like?
I believe that technology and patient care are coming together to create a proactive, predictive and personalised healthcare environment. This evolution will radically improve patient care and patient outcomes, setting a new standard of care around the world.






